As 2026 begins, big insurers like UnitedHealth, CVS Health, and Molina look more financially comfortable than they did a year ago. One reason is that the extra government help that kept insurance prices lower has now ended.
With that support gone, many people who buy plans on the public marketplaces are likely to see their monthly bills rise. That change eases pressure on insurers’ margins, even as it makes coverage more expensive for millions of households.
ACA Premiums Set To Double In 2026 and Why It’s Bad
Health insurance stocks have started the year on a positive note. Companies like UnitedHealth, CVS, and Molina have posted gains on each trading day so far in 2026.
UnitedHealth has climbed to its highest point in several months, CVS is close to levels it hasn’t seen since late last year, and Molina is trading at its strongest point in weeks. That optimism on Wall Street comes at a cost elsewhere.
The extra financial help that was rolled out during the pandemic made insurance cheaper and opened the door to more people. Now that it’s gone, a larger share of the cost falls back on buyers. And that’s bringing new worries about whether some people will drop their coverage.
What Rising ACA Premiums Mean for Families
A few years back, new credits limited how expensive marketplace plans could get and made some coverage free for people on tighter budgets. Those protections are no longer in place. As a result, many households using the exchanges are likely to see their insurance payments rise steeply this year.
In 2025, roughly 24 million people were enrolled in ACA marketplace plans. More than nine out of ten of them were getting some form of financial support. This is based on reporting from Bloomberg. That’s a big change from 2020, when enrollment sat closer to 11 million.
Since the extra subsidies are now gone, that growth is expected to reverse. Fewer people are likely to keep their coverage as costs rise, and that shift changes who remains in the insurance pool. Over time, that can make the market smaller, older, and riskier for insurers to manage.
Insurers Are Better Positioned Than Patients
If marketplace enrollment shrinks, some insurers will feel it more than others. Companies that depend heavily on exchange plans are the most exposed. A drop in members would hit their revenue first.
Bigger groups like UnitedHealth and CVS are more insulated. This is because their earnings also come from employer plans, public programs, and pharmacy services rather than from the exchanges alone.
Some insurers lean heavily on ACA plans. That group includes Molina, Centene, and Oscar. Their exchange business makes up a large share of what they do.
Others also sell plans on the marketplaces, but it’s a smaller part of their business. UnitedHealth, Elevance, and Cigna fall into that category.
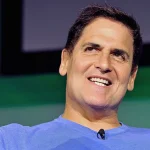
Mark Cuban Calls Insurers Too Big To Care
As these changes play out, Mark Cuban weighed in online. He said rising deductibles are pushing people to cover the full cost of expensive drugs for longer. That can add up to thousands of extra dollars each year for some patients.
Cuban said the money from those pricing deals usually ends up with large middlemen tied to insurers. Meanwhile, patients who need the most care pay more out of pocket. He summed it up by saying the system has grown so large that it no longer serves people well.
On January 7, 2026, Mark wrote on X. He said: “This is your reminder that all those people who had to switch to lower premium, higher deductible plans, will now be paying full retail price on their brand and specialty drugs for LONGER, because their deductibles went up, costing them thousands of dollars a year more.
In aggregate, patients may be paying billions of dollars MORE!
To make matters worse, for your ACA PLANS, the rebates from those deductible buys are going to the biggest PBMs, owned by the insurance companies.
FOR YOUR COMPANY’S plan, if your deductible went up, and it probably did, the in-deductible rebates are going right to your Company’s and the PBM’s BANK ACCOUNT!!!
The bigger your deductible, the sicker you are, the more that goes to your CEO’s balance sheet.
It’s time to change healthcare
These healthcare companies are TOO BIG TO CARE.”
The Political Divide Over Subsidies
Most Democrats support bringing the extra subsidies back. Republicans are more divided. Critics also point to the cost, which is estimated at over $300 billion spread across a decade.
Some lawmakers from both parties back the idea. Public opinion also leans in favor of keeping the help in place. Even so, neither Congress nor the White House has moved to reinstate it so far. Those disagreements directly affect whether millions keep coverage.
Mark Cuban and The Future of Healthcare
What happens next matters less for stock charts and more for real people. The policy choices being delayed now will shape who can stay insured, who drops out, and how heavy the burden feels for families already stretched thin. That’s the part Mark Cuban keeps pointing to. Not the numbers, but the people behind them.
The system has been breaking and deteriorating into something narrower, costlier, and harder to navigate. Whether that drift gets corrected or locked in will define what healthcare looks like for the rest of the decade.